Is fromm linked to heart disease
Heart disease
Overview
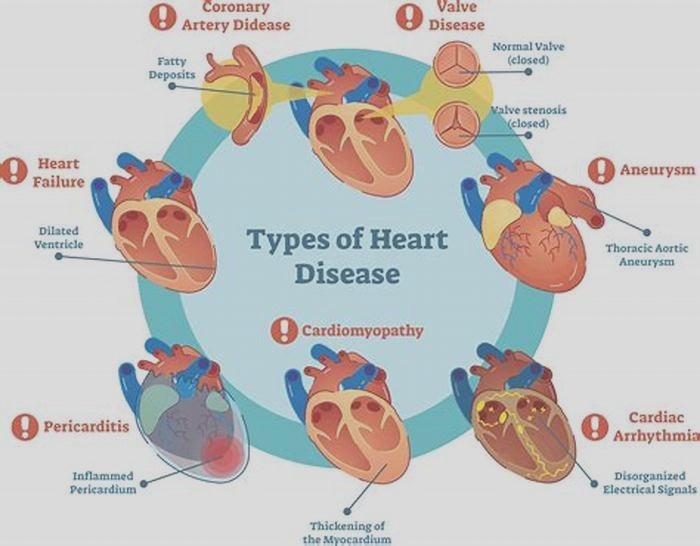
Heart disease describes a range of conditions that affect the heart. Heart diseases include:
- Blood vessel disease, such as coronary artery disease
- Irregular heartbeats (arrhythmias)
- Heart problems you're born with (congenital heart defects)
- Disease of the heart muscle
- Heart valve disease
Many forms of heart disease can be prevented or treated with healthy lifestyle choices.
Products & Services
Symptoms
Heart disease symptoms depend on the type of heart disease.
Symptoms of heart disease in the blood vessels
Coronary artery disease is a common heart condition that affects the major blood vessels that supply the heart muscle. Cholesterol deposits (plaques) in the heart arteries are usually the cause of coronary artery disease. The buildup of these plaques is called atherosclerosis (ath-ur-o-skluh-ROE-sis). Atherosclerosis reduces blood flow to the heart and other parts of the body. It can lead to a heart attack, chest pain (angina) or stroke.
Coronary artery disease symptoms may be different for men and women. For instance, men are more likely to have chest pain. Women are more likely to have other symptoms along with chest discomfort, such as shortness of breath, nausea and extreme fatigue.
Symptoms of coronary artery disease can include:
- Chest pain, chest tightness, chest pressure and chest discomfort (angina)
- Shortness of breath
- Pain in the neck, jaw, throat, upper belly area or back
- Pain, numbness, weakness or coldness in the legs or arms if the blood vessels in those body areas are narrowed
You might not be diagnosed with coronary artery disease until you have a heart attack, angina, stroke or heart failure. It's important to watch for heart symptoms and discuss concerns with your health care provider. Heart (cardiovascular) disease can sometimes be found early with regular health checkups.
What is coronary artery disease? A Mayo Clinic cardiologist explains.
Stephen Kopecky, M.D., talks about the risk factors, symptoms and treatment of coronary artery disease (CAD). Learn how lifestyle changes can lower your risk.
{Music playing}
Stephen Kopecky, M.D., Cardiovascular Disease, Mayo Clinic: I'm Dr. Stephen Kopecky, a cardiologist at Mayo Clinic. In this video, we'll cover the basics of coronary artery disease. What is it? Who gets it? The symptoms, diagnosis and treatment. Whether you're looking for answers for yourself or someone you love, we're here to give you the best information available.
Coronary artery disease, also called CAD, is a condition that affects your heart. It is the most common heart disease in the United States. CAD happens when coronary arteries struggle to supply the heart with enough blood, oxygen and nutrients. Cholesterol deposits, or plaques, are almost always to blame. These buildups narrow your arteries, decreasing blood flow to your heart. This can cause chest pain, shortness of breath or even a heart attack. CAD typically takes a long time to develop. So often, patients don't know that they have it until there's a problem. But there are ways to prevent coronary artery disease, and ways to know if you're at risk and ways to treat it.
Who gets it?
Anyone can develop CAD. It begins when fats, cholesterols and other substances gather along the walls of your arteries. This process is called atherosclerosis. It's typically no cause for concern. However, too much buildup can lead to a blockage, obstructing blood flow. There are a number of risk factors, common red flags, that can contribute to this and ultimately lead to coronary artery disease. First, getting older can mean more damaged and narrowed arteries. Second, men are generally at a greater risk. But the risk for women increases after menopause. Existing health conditions matter, too. High blood pressure can thicken your arteries, narrowing your blood flow. High cholesterol levels can increase the rate of plaque buildup. Diabetes is also associated with higher risk, as is being overweight. Your lifestyle plays a large role as well. Physical inactivity, long periods of unrelieved stress in your life, an unhealthy diet and smoking can all increase your risk. And finally, family history. If a close relative was diagnosed at an early age with heart disease, you're at a greater risk. All these factors together can paint a picture of your risk for developing CAD.
What are the symptoms?
When coronary arteries become narrow, the heart doesn't get enough oxygen-rich blood. Remember, unlike most pumps, the heart has to pump its own energy supply. It's working harder with less. And you may begin to notice these signs and symptoms of pressure or tightness in your chest. This pain is called angina. It may feel like somebody is standing on your chest. When your heart can't pump enough blood to meet your body's needs, you might develop shortness of breath or extreme fatigue during activities. And if an artery becomes totally blocked, it leads to a heart attack. Classic signs and symptoms of a heart attack include crushing, substernal chest pain, pain in your shoulders or arms, shortness of breath, and sweating. However, many heart attacks have minimal or no symptoms and are found later during routine testing.
How is it diagnosed?
Diagnosing CAD starts by talking to your doctor. They'll be able to look at your medical history, do a physical exam and order routine blood work. Depending on that, they may suggest one or more of the following tests: an electrocardiogram or ECG, an echocardiogram or soundwave test of the heart, stress test, cardiac catheterization and angiogram, or a cardiac CT scan.
How is it treated?
Treating coronary artery disease usually means making changes to your lifestyle. This might be eating healthier foods, exercising regularly, losing excess weight, reducing stress or quitting smoking. The good news is these changes can do a lot to improve your outlook. Living a healthier life translates to having healthier arteries. When necessary, treatment could involve drugs like aspirin, cholesterol-modifying medications, beta-blockers, or certain medical procedures like angioplasty or coronary artery bypass surgery.
What now?
Discovering you have coronary artery disease can be overwhelming. But be encouraged. There are things you can do to manage and live with this condition. Reducing cholesterol, lowering blood pressure, quitting tobacco, eating healthier, exercising and managing your stress can make a world of difference. Better heart health starts by educating yourself. So don't be afraid to seek out information and ask your doctors about coronary artery disease. If you'd like to learn even more about this condition, watch our other related videos or visit Mayoclinic.org. We wish you well.
Heart disease symptoms caused by irregular heartbeats (heart arrhythmias)
The heart may beat too quickly, too slowly or irregularly. Heart arrhythmia symptoms can include:
- Chest pain or discomfort
- Dizziness
- Fainting (syncope) or near fainting
- Fluttering in the chest
- Lightheadedness
- Racing heartbeat (tachycardia)
- Shortness of breath
- Slow heartbeat (bradycardia)
Heart disease symptoms caused by congenital heart defects
Serious congenital heart defects usually are noticed soon after birth. Congenital heart defect symptoms in children could include:
- Pale gray or blue skin or lips (cyanosis)
- Swelling in the legs, belly area or areas around the eyes
- In an infant, shortness of breath during feedings, leading to poor weight gain
Less-serious congenital heart defects are often not diagnosed until later in childhood or during adulthood. Symptoms of congenital heart defects that usually aren't immediately life-threatening include:
- Easily getting short of breath during exercise or activity
- Easily tiring during exercise or activity
- Swelling of the hands, ankles or feet
Heart disease symptoms caused by diseased heart muscle (cardiomyopathy)
Early stages of cardiomyopathy may not cause noticeable symptoms. As the condition worsens, symptoms may include:
- Dizziness, lightheadedness and fainting
- Fatigue
- Feeling short of breath during activity or at rest
- Feeling short of breath at night when trying to sleep or waking up short of breath
- Irregular heartbeats that feel rapid, pounding or fluttering
- Swollen legs, ankles or feet
Heart disease symptoms caused by heart valve problems (valvular heart disease)
The heart has four valves the aortic, mitral, pulmonary and tricuspid valves. They open and close to move blood through the heart. Many things can damage the heart valves. A heart valve may become narrowed (stenosis), leaky (regurgitation or insufficiency) or close improperly (prolapse).
Valvular heart disease is also called heart valve disease. Depending on which valve isn't working properly, heart valve disease symptoms generally include:
- Chest pain
- Fainting (syncope)
- Fatigue
- Irregular heartbeat
- Shortness of breath
- Swollen feet or ankles
Endocarditis is an infection that affects the heart valves and inner lining of the heart chambers and heart valves (endocardium). Endocarditis symptoms can include:
- Dry or persistent cough
- Fever
- Heartbeat changes
- Shortness of breath
- Skin rashes or unusual spots
- Swelling of the legs or belly area
- Weakness or fatigue
When to see a doctor
Seek emergency medical care if you have these heart disease symptoms:
- Chest pain
- Shortness of breath
- Fainting
Always call 911 or emergency medical help if you think you might be having a heart attack.
Heart disease is easier to treat when detected early. Talk to your health care provider if you have any concerns about your heart health. Together, you and your provider can discuss ways to reduce your heart disease risk. This is especially important if you have a family history of heart disease.
If you think you may symptoms of heart disease, make an appointment to see your provider.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
ErrorEmail field is required
ErrorInclude a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Causes
Heart disease causes depend on the specific type of heart disease. There are many different types of heart disease.
How the heart works
Chambers and valves of the heart
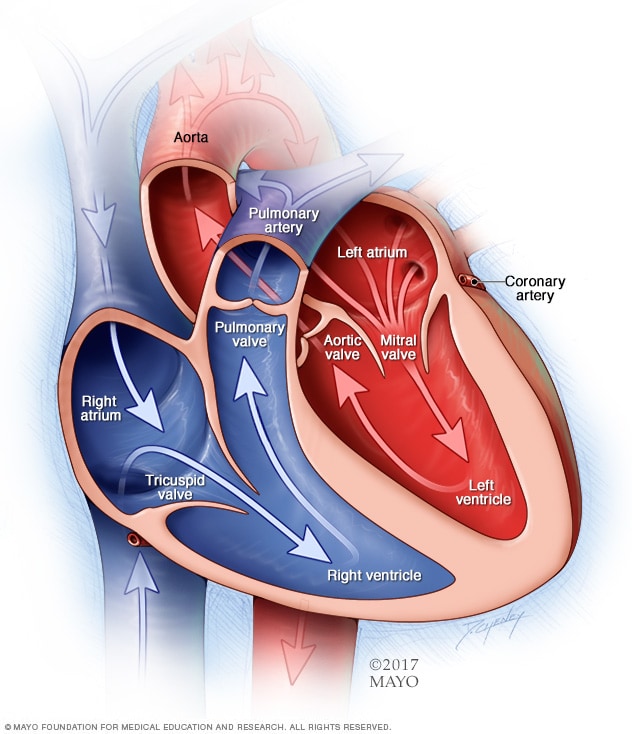
Chambers and valves of the heart
A typical heart has two upper and two lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of the heart. The heart valves, which keep blood flowing in the right direction, are gates at the chamber openings.
To understand the causes of heart disease, it may help to understand how the heart works.
- The heart is divided into chambers two upper chambers (atria) and two lower chambers (ventricles).
- The right side of the heart moves blood to the lungs through blood vessels (pulmonary arteries).
- In the lungs, blood picks up oxygen and then returns to the left side of the heart through the pulmonary veins.
- The left side of the heart then pumps the blood through the aorta and out to the rest of the body.
Heart valves
Four heart valves the aortic, mitral, pulmonary and tricuspid keep the blood moving the right way. The valves open only one way and only when they need to. Valves must open all the way and close tightly so there's no leakage.
Heartbeats
A beating heart squeezes (contracts) and relaxes in a continuous cycle.
- During contraction (systole), the lower heart chambers (ventricles) squeeze tight. This action forces blood to the lungs and the rest of the body.
- During relaxation (diastole), the ventricles fill with blood from the upper heart chambers (atria).
Electrical system
The heart's electrical system keeps it beating. The heartbeat controls the continuous exchange of oxygen-rich blood with oxygen-poor blood. This exchange keeps you alive.
- Electrical signals start in the upper right chamber (right atrium).
- The signals travel through specialized pathways to the lower heart chambers (ventricles). This tells the heart to pump.
Causes of coronary artery disease
Development of atherosclerosis
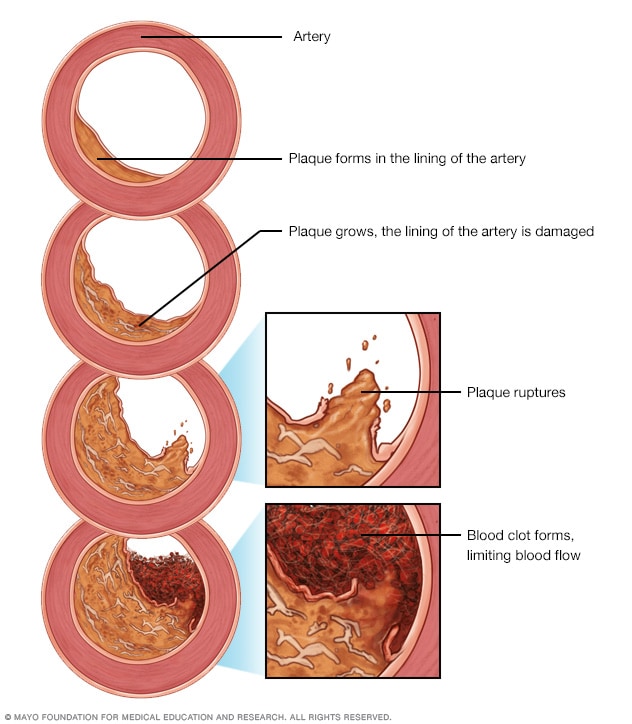
Development of atherosclerosis
If there's too much cholesterol in the blood, the cholesterol and other substances may form deposits called plaque. Plaque can cause an artery to become narrowed or blocked. If a plaque ruptures, a blood clot can form. Plaque and blood clots can reduce blood flow through an artery.
A buildup of fatty plaques in the arteries (atherosclerosis) is the most common cause of coronary artery disease. Risk factors include a poor diet, lack of exercise, obesity and smoking. Healthy lifestyle choices can help lower the risk of atherosclerosis.
Causes of irregular heartbeats (arrhythmias)
Common causes of arrhythmias or conditions that can lead to them include:
- Cardiomyopathy
- Coronary artery disease
- Diabetes
- Drug misuse
- Emotional stress
- Excessive use of alcohol or caffeine
- Heart problem present at birth (congenital heart defects)
- High blood pressure
- Smoking
- Heart valve disease
- Use of certain medications, including those bought without a prescription, and herbs and supplements
Causes of congenital heart defects
A congenital heart defect develops while a baby is growing in the womb. A congenital heart defect forms as the baby's heart develops, about a month after conception. Congenital heart defects change the flow of blood in the heart. Some medical conditions, medications and genes increase the risk of congenital heart defects.
Causes of a thickened or enlarged heart muscle (cardiomyopathy)
The cause of cardiomyopathy depends on the type:
- Dilated cardiomyopathy. The cause of this most common type of cardiomyopathy often is unknown. It may be passed down through families (inherited). Dilated cardiomyopathy typically starts in the heart's main pumping chamber (left ventricle). Many things can cause damage to the left ventricle, including heart attacks, infections, toxins and some drugs, including cancer medicines.
- Hypertrophic cardiomyopathy. This type is usually passed down through families (inherited).
- Restrictive cardiomyopathy. This is the least common type of cardiomyopathy. It can occur for no known reason. Sometimes it's caused by a buildup of protein called amyloid in the heart (cardiac amyloidosis) or connective tissue disorders.
Causes of heart infection
A heart infection, such as endocarditis, occurs when germs reach the heart or heart valves. The most common causes of heart infections are:
- Bacteria
- Viruses
- Parasites
Causes of heart valve disease
Many things can cause diseases of the heart valves. Some people are born with heart valve disease (congenital heart valve disease). Heart valve disease may also be caused by conditions such as:
- Rheumatic fever
- Infections (infectious endocarditis)
- Connective tissue disorders
Risk factors
Risk factors for heart disease include:
- Age. Growing older increases the risk of damaged and narrowed arteries and a weakened or thickened heart muscle.
- Sex. Men are generally at greater risk of heart disease. The risk for women increases after menopause.
- Family history. A family history of heart disease increases the risk of coronary artery disease, especially if a parent developed it at an early age (before age 55 for a male relative, such as your brother or father, and 65 for a female relative, such as your mother or sister).
- Smoking. If you smoke, quit. Substances in tobacco smoke damage the arteries. Heart attacks are more common in smokers than in nonsmokers. If you need help quitting, talk to your health care provider about strategies that can help.
- Unhealthy diet. Diets high in fat, salt, sugar and cholesterol have been linked to heart disease.
- High blood pressure. Uncontrolled high blood pressure can cause the arteries to become hard and thick. These changes interrupt blood flow to the heart and body.
- High cholesterol. Having high cholesterol increases the risk of atherosclerosis. Atherosclerosis has been linked to heart attacks and strokes.
- Diabetes. Diabetes increases the risk of heart disease. Obesity and high blood pressure increase the risk of diabetes and heart disease.
- Obesity. Excess weight typically worsens other heart disease risk factors.
- Lack of exercises. Being inactive (sedentary lifestyle) is associated with many forms of heart disease and some of its risk factors, too.
- Stress. Unrelieved stress may damage the arteries and worsen other risk factors for heart disease.
- Poor dental health. It's important to brush and floss your teeth and gums often. Also get regular dental checkups. Unhealthy teeth and gums makes it easier for germs to enter the bloodstream and travel to the heart. This can cause endocarditis.
Complications
Complications of heart disease include:
- Heart failure. This is one of the most common complications of heart disease. Heart failure occurs when the heart can't pump enough blood to meet the body's needs.
- Heart attack. A heart attack may occur if a blood clot is stuck in a blood vessel that goes to the heart.
- Stroke. The risk factors that lead to heart disease can also lead to an ischemic stroke. This type of stroke happens when the arteries to the brain are narrowed or blocked. Too little blood reaches the brain. A stroke is a medical emergency brain tissue begins to die within just a few minutes of a stroke.
- Aneurysm. An aneurysm is a bulge in the wall of an artery. If an aneurysm bursts, you may have life-threatening internal bleeding.
- Peripheral artery disease. In this condition, the arms or legs usually the legs don't get enough blood. This causes symptoms, most notably leg pain when walking (claudication). Atherosclerosis can lead to peripheral artery disease.
- Sudden cardiac arrest. Sudden cardiac arrest is the sudden loss of heart function, breathing and consciousness. It's usually due to a problem with the heart's electrical system. Sudden cardiac arrest is a medical emergency. If not treated immediately, it results in sudden cardiac death.
Prevention
The same lifestyle changes used to manage heart disease may also help prevent it. Try these heart-healthy tips:
- Don't smoke.
- Eat a diet that's low in salt and saturated fat.
- Exercise at least 30 minutes a day on most days of the week.
- Maintain a healthy weight.
- Reduce and manage stress.
- Control high blood pressure, high cholesterol and diabetes.
- Get good sleep. Adults should aim for 7 to 9 hours daily.
More Information
Aug. 25, 2022